Introduction
Going back to clinical discussion, as per my prior article. Although not highly common, I see this issue as a rheumatologist not uncommonly. Sorry for the last sentence but the level of vagueness is necessary to be accurate. I get occasionally patients that have mechanical/osteoarthritis/fibromyalgia like pains. The kicker is that they are younger than 40 years old and with no heavy labor history. The interesting point that these patients mention how naturally flexible they were as kids, and possibly till now, with some to degree of dislocating joints.
Although there is a long list of flexibility disease, a lot of them have prominent physical features that let you suspect that they are not healthy except 2 (that I know of). One is called Ehlers Danlos Syndrome type IV, which I have suspected once. Typically, these patients have personal or family history of blood vessel aneurysm (blood vessel swells up as its walls thins) or internal organs ruptures such as uterus rupture during delivery of babies. I also suspect it when patients have history of sudden death in the family that is unexplained.
The other disease I suspect and see more commonly is called Ehlers Danlos Syndrome type III. These people don’t have internal organ issues, but usually have double jointness which doctors call benign hyper-flexibility syndrome. They might have a bit of stretchy skin. (look link below from a nice article).
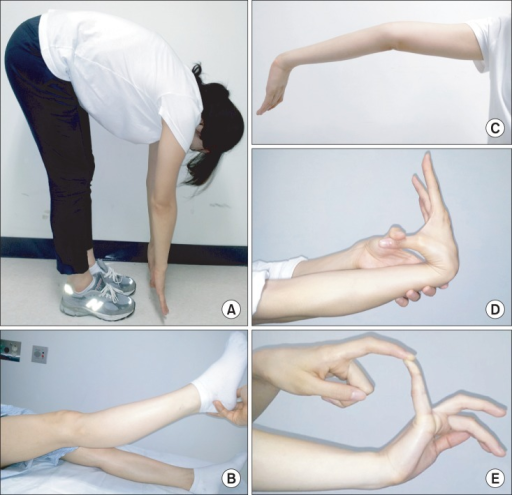
Main way to diagnose benign hypermobility syndrome
The way we figure out if you have this issue, is examination. I was initially wanted to go on a whim of explaining each exam but this website has awesome picture of how we do it. “Doc, then what are you going to talk about?”. I will talk about what the patient is feeling through life stages. I kind of noted them clinically, but I was happy to see an expert writing a beautiful research article describing what I noted in my clinic. I will summarize it here.
Classical symptoms progression of benign hypermobility syndrome.
In the first few years of life, the person might experience ability to flatten their hands on the floor when they bend their torso but also, they would could get dislocation and joint injuries easier than their peers. Also, repetitive tasks like writing could prove painful. Then these individuals, in their 20’s to 40s, could move to a pain stage which emulates fibromyalgia with diffuse pains, headaches, and pelvic pain (in women). At this stage, they might feel tingling sensations, fainting sensation when standing up from sitting position (orthostatic hypotension), abdominal pains, and pelvis pains.
Also from my experience, they describe a condition similar to Raynaud’s but the usual difference that it is not cold specific as in Raynaud’s. At times though, it is hard to differentiate and most doctors could confuse the 2. The nerves that control blood vessels, we call autonomic nerves, gets somehow affected due to the connective tissue structure issues. These autonomic nerves seem more sensitive than sensation/feeling/touch nerves. Note that diabetics can get autonomic nerve symptoms commonly too. Final stage of the disease would be stiffness from the chronic pain and damage over the years. Interestingly, I have seen in clinic, despite stiffness complaints, these patients are more flexible than I am.
Additional symptoms of benign hypermobility syndrome?
Other symptoms you can see in benign hypermobility syndrome are:
1)stretchy fragile skin (see this article pictures)
2) Orthostatic hypotension (discussed above already) or POTS (Postural tachycardia syndrome). The latter described as increased heart rate that happens to compensate for blood pressure drop.
3) Possibly the root of the aorta (large blood vessel from the heart feeding the rest of the body) could be dilated but echocardiogram is not always recommended as screening.
4) Jaw joint called temporomandibular joint could have pains. Usually, oromaxillofacial surgeon is best to evaluate. Which is a special kind of dentists.
5) heavy menstrual bleeding
6) Urinary incontinence (inability to hold urine and it starts dripping) or pelvic organ prolapse (the uterus for example is lower and can lead to pains). Usually, specialized gynecologist can do surgery for these.
When referral to medical genetics is likely a must for hypermobility syndrome
In general, the one to confirm diagnosis is a medical genetics doctor. Rheumatologist know about the disease because we deal with pain. If you do not know, most patients want explanation for their pains from my experience. The issue with medical genetics that they are less available even less than Rheumatologists. Also, they sometime subspecialize to deal with subset of genetic disease such as familial cancers or just vascular complicated, such as blood vessel rupture, connective tissue disease. Therefore, from my experience it is hard to get a referral. That is why, it is important to educate patients and primary provider about the issue.
Summary
I hope this article on benign hypermobility syndrome just helps you sort out your pains. One sentence on management. Management is focused on the symptoms to be managed based on respective specialty. For example, abdominal pain ==> GI, pelvic pain==> gynecology, POTS==> cardiology or neurology, pain==> pain clinic, osteoarthritis ==> Physical therapy, Rheumatology, and orthopedics. I wish best of luck on your life journey
Resources:
https://onlinelibrary.wiley.com/doi/pdf/10.1002/ajmg.c.31538
https://www.hypermobility.org/what-is-hypermobility simplified website but I have not delved to all points mentioned to verify them. Go on your own risk.
https://www.ehlers-danlos.com/assessing-joint-hypermobility/ Test your mobility or hypermobility
https://onlinelibrary.wiley.com/doi/pdf/10.1002/ajmg.c.31538 Nice picture to explain stretchy skin
Kwon JW, Lee WJ, Park SB, Kim MJ, Jang SH, Choi CK -Annals of rehabilitation medicine(2013) https://creativecommons.org/licenses/by-nc/3.0/



