Who should read the lupus diagnosis article?
Before I answer this question, the answer is mainly for people who never had biopsy (from the kidney for example). This question might not be helpful to people who have been seeing a Rheumatologist for 2 or more years.
Lupus diagnosis the Rheumatological disease archetype
Why does this question matter for Rheumatologist? Generally, Rheumatologist are trained on lupus as an archetype disease. Meaning the way we diagnose lupus; we use it to diagnose other autoimmune diseases. Somehow through the history of medicine some health care providers ignored the fact that lupus is a disease diagnosed clinically. Diagnosis of lupus was a prime example of how good history and exam can help find a quite elusive disease. With the advent of blood testing, health care providers sometimes act as if they forgot the fact. Instead of patients being investigated systematically, a test is thrown at the patient.
Positive lupus labs without lupus diagnosis
What happens is that patients with positive labs, even if they do not have autoimmune disease get referred to a Rheumatologist. AND patients with autoimmune disease that have negative testing, get delayed diagnosis. At times the thing being tested is good but the way it is being tested is wrong. The last piece is usually known by the specialist and might take time to explain to generalists and the general population. BUT clinical history is what matters the most.
Likelihood of lupus diagnosis
Let us talk about lupus diagnosis as this is the concern for most patients with positive labs in my clinic. To be assured, most patients referred to for question lupus, do NOT even have a rheumatological autoimmune disease. Of those with positive “lupus test” and do have autoimmune disease, it might not be lupus. Of those with lupus diagnosis, only a small fraction has aggressive disease.
Lupus diagnosis with negative labs!?
However, before I move forward, let me say this. For the purpose of generalist (primary care providers) and patients, there are no lupus patients with negative Antinuclear antibody by Immunofluorescence. This is more so if a Rheumatologists evaluated you and said your ANA is negative when it is marked red by the computer system. Rheumatologists understand levels of test, while in general other specialists and primary care providers do not understand it quite well.
How to search for lupus diagnosis
As a Rheumatologist how do I search for lupus? I kind of do not. I dissect each of your symptoms then categorize in my brain as completely unrelated and to be ignored (from lupus diagnosis perspective only as I still help the patient manage it) or potentially autoimmune related. I try my best to ignore medical names. I have been told by patients: “my doctor told me I have lupus as I have malar rash, Raynaud’s, inflammation in my joints, and nephritis; therefore, I have lupus”. On closer analysis I realized that the patient has Rosacea, cyanosis, osteoarthritis, and diabetic nephropathy”. This scenario is insanely common.
Initial steps in evaluating lupus diagnosis
Let me take you on a tour of my mind. I start by looking in the patient chart at the age. Immediately if I see a patient above 50, the case of autoimmune disease reduces. It does not disappear but drops. The probability even drops much more if the patient is 70-year-old or more. This is based on probabilities we know. Then I go to the pain questions. “Where are you hurting?” As you saw in prior articles, for lupus (or any rheumatological autoimmune disease) I expect pains to be in joints specifically and not spanning muscle groups, skin, or bone. I expect pain to be 2-4 hours in the morning with inability to move the joint involved. I expect the patient did NOT have trauma to that joint. That gives me point 1, possible autoimmune joint disease.
Lupus rash?
Then I go to rashes. If you have a diagnosed rash such as eczema of psoriasis, obviously I jump to this question. If you do have a non-diagnosed recurrent rash, I ask does it gets worse with the sun mainly. It gets worse with heat, spicey food, stress, or other reasons I might not count the rash. If the rash is itchy, I am unlikely to count the rash. If you have a dermatologist, tell you based on biopsy this is eczema “as an example”, I will not count the rash.
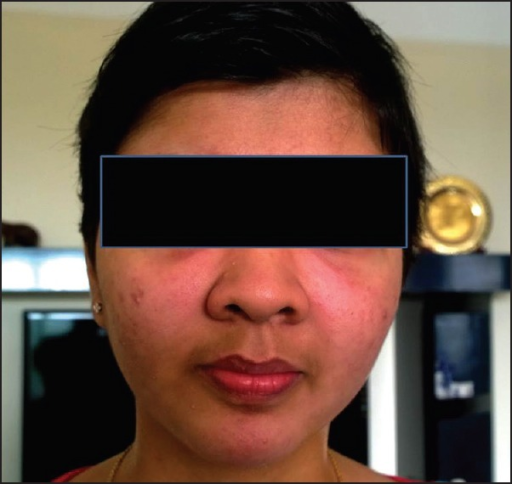
Lupus face rash?
Spinning of this topic, I will talk malar rash. Lupus malar rash is overly diagnosed and is not a good sign even in hands of a Rheumatologist based on specificity studies – study that determines when a thing (test or symptom) is there, what is the likelihood it means you have a disease. But that rash does NOT involve your forehead nor chins. Malar rash is NOT itchy. Malar rash does not affect the area between cheeks and nasal flare. Most common rash that gets confused with malar rash is Rosacea “based on what I have seen”. Keep in mind that even when you have a Rheumatologist telling you this is a Malar rash for sure, it is not always a good sign to depend on to diagnose lupus. (1)
Dry mouth, eyes, and vaginal area
Then I go to dry eyes, mouth, and vaginal area. If you are diabetic or on several medications for allergies, migraines, blood pressure, and any meds that cause dryness; then I do not count this. When I say dry eyes, I do not mean exaggerated watering or tears. I mean that you can NOT produce tears. Dry mouth means almost a cotton mouth feeling that prevents you from chewing food or from talking without interruption from severe dryness. If you have 2/3 areas above dry without other explanation, I count it as 1 point. Keep in mind, this does not mean lupus, as can be seen in Rheumatoid arthritis, and Sjogren syndrome too. Do not start googling yet.
Hair loss and lupus
I evaluate hair loss cautiously and usually tend to ignore it. My preference is to only include it when there is absence of hair completely which is quite rare. Another instance is when there is absence of hair in an area of quarter coin at least. Usually this is diagnosed by a dermatologist as alopecia areata. I do NOT take the following as true bold spots: patient tugs on their hair to braid it, hairdressers’ comments of bold spot, and feeling of bold spots. I usually want a picture showing a complete desert patch with no plants at all. From my clinical experience, hair loss is an overrated sign of lupus. The reason is that hair is sensitive, and any stressful situation can lead to hair loss such as: nutritional deficiency, thyroid disease, general illness, and even psychological stress. Note, every person loses their hair as they age.
mouth and nose ulcers, are they from lupus diagnosis?
Oral and nose ulcers are good symptoms to use but still you need to keep in mind description. Ulcers are not pimples, general crusting, nor polyps. Regarding lupus oral ulcers, I am looking for inner cheeks or roof of the mouth ulcers that happen without a cause and usually are painless. The ulcers are NOT white with string-like structure –that is lichen planus or fungus. I do NOT count cold sores that occur on lips. Keep in mind nutritional deficiencies can also cause mouth sores. If I see a nose ulcer, I take it seriously as nose ulcers are way less common than mouth ulcers in the population.
Raynaud and lupus diagnosis.
I usually do not ask about Raynaud’s as it is one of the most confusing symptoms. For one, a large section of physicians diagnosed Raynaud’s, is cyanosis. Cyanosis is poor blood flow in the periphery of blood vessels due to lower oxygenation. Cyanosis can even happen in tips of noses but not Raynaud’s. I think even physicians confuse poor blood flow from Raynaud’s. Raynaud’s is a reactionary process that can lead to poor blood flow, but there is tons of reasons for poor blood flow. I start asking any patient with fingers changing color is it only the tips of the finger or whole finger. If only the tips, then this is NOT Raynaud’s. Raynaud’s is a change of the color of the whole finger to blanching white, dark purple, and/or red. Color changes occur at specific cold temperature for the patient, and it is generally painful. Let us say patient is not sure, I dig for poor blood flow and/or poor oxygenation causes. I ask about smoking, asthma, cardiac disease diabetes, high cholesterol, trauma to hands, illicit drug use, migraine medications, blood pressure medications, and repetitive hand irritation (such as jackhammer users). You get the point, if there is no other explanation for blood flow issue, I count one point.
Covering of the heart and lung and lupus.
Serositis. What is that??? The lining covering the outside of the lung (pleura), lining covering the heart (pericardium), and covering the bowel (peritoneum) can be affected un lupus. Usually, however, these patients do not come walking towards the clinic. I see these complaints mainly in admitted lupus patients as usually it occurs during another bad event such as lupus kidney. If they start occurring, they seem to me intolerable for a patient not to go to emergency department. Usually, they are sharp pain that occurs with deep breathing and last for a bout then disappear. We try to find these issues on testing such as chest x-ray, electrocardiogram, and CT of the abdomen. They are quite elusive as most patients who have similar sounding pain have functional syndromes and not lupus such as muscle spasms or irritable bowel syndrome. If your pain can be induced or made worse by pushing on the area, then this is likely a muscle issue. If abdominal pain happens along with diarrhea and/or constipation, then it is likely a functional issue.
Potentially serious and dangerous, But rare
I will move to a category I call “serious dangerous and rare stuff with NO explanation”. This stuff must be evaluated by the proper specialist first then I could consider if they are lupus related or not. I will list the thing, its specialist, and how it could relate to lupus. Keep in mind though that I will create more detailed description in future articles so brevity here is losing some important info.
- Protein and blood in urine testing. Nephrologist (medical doctor of the kidneys). Lupus nephritis.
- Recurrent Miscarriages. Gynecologist. Antiphospholipid syndrome.
- Stroke and heart attacks. Neurologist and cardiologist. Antiphospholipid syndrome.
- Seizure (new). Neurologist. Antiphospholipid syndrome.
Closing remarks
Closing remarks: although these issues are not the only ones but usually, they are the way I diagnose lupus. Unfortunately, I have seen lists even in lupus related organizations that mention symptoms that are not specific to lupus and are so common that they lead to a sea of anxiety among my patients. It is disappointing and disheartening. My goal is not to disparage anyone who complains, my goal is for you to find what is the true reason of your complaints. Although it takes lupus 6 years to diagnose, I do not think the issue is looking for the disease. I receive large numbers of referrals for possible lupus. I believe the issue lies in the poor information circulating distributed by mostly well-intentioned physicians and healthcare journalists BUT a large number of this information is either confusing or at times completely erroneous.
Resources:
Chandra SR, Issac TG, Ayyappan K -Indian journal of psychological medicine(2015 Jul-Sep)




Comments
Pingback: How to treat lupus? Jumpstart guidance - Medical Hermit
Pingback: Pregnancy and autoimmune disease. quick guidance on 3 main issues - Medical Hermit