Introduction
So initial disclaimer on Rheumatological interstitial lung disease and request: do NOT freak out. This article is not to suggesting this is a common issue. I just get referred a LOT of patients with this question. Most patient come anxious and confused. Now I got a knack for breaking it down verbally and walk you through it. As per usual, a doc might tell you “You have autoimmune, go to Rheum”.
I strongly suggest you read my article “What is a Rheumatologist?”, because I get commonly asked “why am I seeing an arthritis doctor?”. Long story short, we are doctors who also manage autoimmune disease that could affect multiple organs. You probably won’t find what I will describe here in a book, at least not the way I arrange it here.
Breathing issue: is it autoimmune interstitial lung disease or something else?
Let me start with saying: even patients with autoimmune disease are likely to have shortness of breath from other disease than autoimmune interstitial lung disease affecting the lung. The reason is simple. Common issues are common. There are vastly more asthma/allergy patients and heart disease patients than autoimmune disease of the lung. The other thing I will say, blood tests does not diagnose autoimmune disease of the lung. “Then doc, what does say if I have autoimmune disease of the lung?” The answer:
- Breathing test called pulmonary function test (PFT)
- An advanced detailed picture of the lung, we call high resolution computed tomography (HRCT)
- Possibly you will need biopsy of questionable area found on HRCT
Pulmonary function test
Let us start with general concept of breathing test (PFT). This tests measures:
- FEV1/FVC which is how much of the air in your lung you can push out on breathing out (exhaling). If this is bad, generally you are thinking asthma/allergy vs COPD (lung disease from smoking)
- FVC percentage which is how much air you can store in your lung. If this is low, you could be thinking heart/kidney failure (if water is filling the bases of the lung), special kind of allergy called hypersensitivity pneumonitis, or my issue of interstitial lung disease. The latter could be an autoimmune issue.
- DLCO which is how much oxygen moves from lung air pockets to blood. If this is abnormal it could be a heart or lung issue. If FVC is normal then it possibly a heart issue requiring echocardiogram or special kind with a bubble study (this sees if there is small whole in heart making oxygen flow unorganized).
What if pulmonary function test is abnormal?
If the breathing test is abnormal then we might need more testing. If FVC is lower than 90 and there is no clear explanation, then we would start with an HRCT. If DLCO is abnormal ALONE with normal FVC percentage, then you likely need as echocardiogram. If you are younger than 40, then a bubble study echo might be a good idea.
Ok now I explained basis of testing. When should autoimmune issue be considered? And what types I see. I will start with one I have more experience with. I have experience with it as I worked in a university that saw that type A LOT. This is not usual. Let us say a person gets short of breath or cough a lot. Their docs will ask if you had any long term (usually work related) exposure to chemicals, fumes, birds, or animals. As that could sway diagnosis. Obviously smoking history is a BIG one.
Then the patient will get some blood tests and PFT. Let us say the PFT FVC was low, the patient will get HRCT. Then either you see issues in the upper part of the lung or basis of the lung. If the upper part of the lung is involved, you are talking chronic allergies or infection. If mostly, or only, base of the lung issue then we are talking entity called interstitial lung disease. Now my job starts.
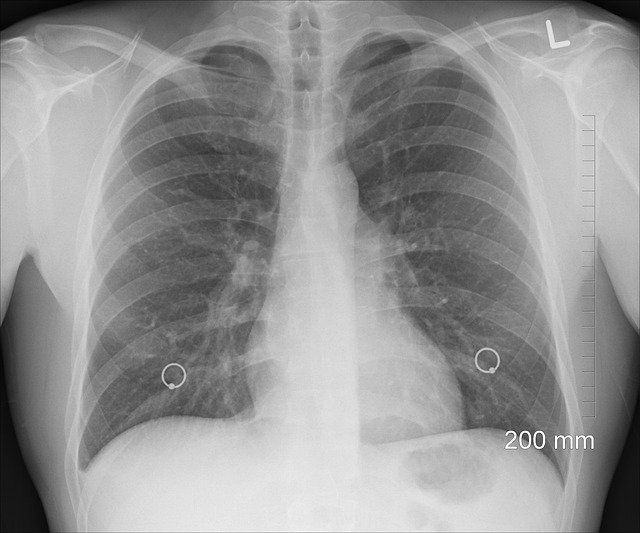
The high resolution CT scan test
It depends what the radiologist describes in the report. If the base of the lung shows ground glass opacities and patient has no history of heart nor kidney disease then you are thinking:
- Atelectasis can happen with old age and after infection but If FVC on PFT is abnormal we think of number 2, discussed below, as it is more serious. Especially if patient did not have history of recent infection. Note if a patient just got out of the hospital due to pneumonia or heart failure, then this could be due to that.
- Interstitial lung disease, namely something called non-specific interstitial pneumonitis. The radiologist would say that in the final impression on their report.
Radiologist impression or judgement on the CT
If the radiologist says, “Usual interstitial pneumonia”, honeycombing, traction bronchiectasis, or traction bronchiectasis THEN I also consider autoimmune rheumatological issues as a possibility. Keep in mind smoking history and chemical exposures could be reason.
Now we end up with 2 entities that a Rheumatologist might help with:
- NSIP: this is more of active autoimmune issue that Rheumatologist can help with
- UIP: this is more of old damage or fibrosis that lung doc can help with a group of meds called antifibrotic.
Why see a Rheumatologist?
Both needs Rheumatologist evaluation as if there are other underlying disease, they might require special monitoring. But keep in mind that a lot of patients specially UIP do NOT have a rheumatological disease. What about NSIP? This is a special one. Even in absence of a rheumatological disease that is clear, these patients could benefit from drugs Rheumatologist prescribe such as Rituximab and/or Mycophenolate Mofetil. Do all patients needs drugs? It depends on initial FVC from PFT and/or comparison with repeat one in 3-6 months. As if changes are stable for 6 months, you are likely dealing with atelectasis not NSIP. If FVC is getting worse, and lung doctor ruled out infections reasonably, then it is likely NSIP.
Due to this article being long, I elected to talk about ball like lesions on CT scans, and their possible (relatively rare) connection to rheumatological autoimmune issues, in another article.

Laria A, Lurati A, Scarpellini M -Case reports in rheumatology(2015) https://creativecommons.org/licenses/by/3.0/



Comments
Pingback: Sarcoid granuloma and ANCA granuloma: quick guidance on 1 Ball like lesion lung disease - Medical Hermit