What are joints?
Before talking about why your joints are hurting, what are joints. So, the word joints might be more confusing than most people think. To simplify, whatever bends in your body is a joint. You or your providers might confuse you more by saying that google says that the skull has joints, but they do not have visible movements as adults. My goal in this blog is to simplify and not to be overly academic. So back to our bendy theory. If it bends in predictable manner; it is a joint.
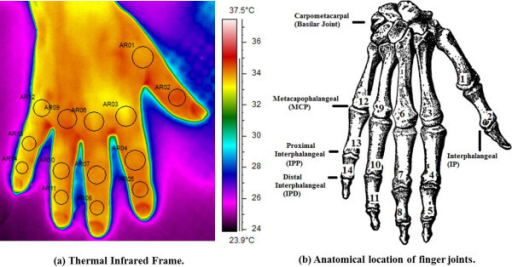
Let’s list them in an easy way: far knuckles of the hands(DIP), middle knuckles of the hands(PIP), knuckles where fingers attach to your hands(MCP), base of the thumb joint(CMC), wrists(there is internally few joints there), elbows, shoulders, neck(cervical spine), middle of the back(thoracic spine), lower back (lumbar spine), buttocks(SI joint), hips (femoroacetabular joint, pain felt in groin), knees, ankles, knuckles where toes attach to foot (MTP), foot middle knuckles(PIP), and feet far knuckles(DIP). The acronym you see, after each joint I mentioned, is what docs call these joints. A lot of them can be injected with steroids to relieve pain.
Most common joint issue.
If the joints are hurting you, what do you have? The most common answer is osteoarthritis, which is joint damage from wear and tear. In general, the way to slow down this issue is diet, exercise, and physical therapy. The role of docs (I am using as synonym for health care provider) is to help you relieve pain. We could give you pain pills from different categories. Or we can inject these joints with steroids. There is other new stuff that can be injected depending on the joint such as hyaluronic acid injections into knees. Also, some other newer options (not covered by insurance companies) can also be injected.
I will have more discussion on that matter in dedicated articles. “But do I have other types of arthritis or joint pains?”. Osteoarthritis pains occur typically in patients in their 50’s from my experience. However, could occur at a much younger age even in people in their 20’s. The older we get, the more advanced it gets. The pain and swelling typically get worse as the day progress.
When osteoarthritis has been there for a while, people could have problem moving the joint in the beginning of the day. For example, if it is affecting the hand, then the person won’t be able to open and close the hand completely for 30 min up to 1 hour. “But doc How to know if I don’t have something else?”
Is it wear & tear vs autoimmune?
Either you have something that makes osteoarthritis faster like inherited over flexibility issues OR you have autoimmune disease that is attacking the joints. Typically, we start thinking about these issues if the patient is younger than 50 or especially 40 years old. My goal as a Rheumatologist to find if you have autoimmune disease attacking the joint. I have three main questions:
- How long does it take you to move the joints to your typical flexibility range? For example, if you can typically move your knee to completely be straight or 10 degrees less, how long does it take you to reach that range? If it is 1 hour or more, then this makes me think autoimmune.
- When you wake up after a long rest (NOT end of the day?), is that joint swollen more than your average through the day? If yes, then I think autoimmune.
- Does movement make your pain less most of the time? If yes, then I think autoimmune.
Age and types of autoimmune joint disease
If 2/3 of the above makes me think you have autoimmune, I consider sending some work up based on few other questions I ask and demographics. For example, young males commonly have gout or Rheumatoid arthritis. In young females, I think of lupus, even if patient has no lupus symptoms just because women get more lupus compared to males. We are going to the probability game I talked about in my introduction articles.
Osteoarthritis of the young
“But doc, I answered no to all of the above and I am 26, how come I have osteoarthritis?” three common issues I see in clinic could be the answer. The first reason is hyperflexible syndromes. These typically are not dangerous, but you are so flexible that your tendons and ligaments (ropes that keep joints in check) are not doing a perfect job. Your solution is muscle strengthening, preferably after getting advice from a physical therapist.
The second reason is very intensive physically demanding jobs such as construction workers, gardeners, warehouse workers, nurses (especially in nursing homes and dialysis centers), and hairdressers. The third reason is quite super rare to which I have diagnosed one case 2014 through 2024. It is inherited iron storage disease we call hemochromatosis.
Sudden crazy pain
“But doc, I have one joint swollen and painful to the degree of tears that I cannot lay a bedsheet on it?” “This happens for a week then goes away?” You might be part of special group of gout/pseudogout, especially if you are male, have kidney issues, or older in age.
Where to go from here?
If this article makes you think you have osteoarthritis, I will have a few articles about osteoarthritis, its complications, and how to manage it. If you are thinking of autoimmune disease and you are male, start with Rheumatoid arthritis and gout articles. If you are thinking autoimmune disease and female, you consider reading about Rheumatoid arthritis and lupus. If Rheumatoid arthritis, lupus, and gout articles do not fit you, think of reactive arthritis, infections, or pseudogout.
Resources:
Ismail E, Capo A, Amerio P, Merla A -Biomedical engineering online(2014) https://creativecommons.org/publicdomain/zero/1.0/




Comments
Pingback: I have autoimmune arthritis but which kind (lupus, Rheumatoid, psoriatic…etc.) - Medical Hermit
Pingback: My body is hurting, a useful efficient guide - Medical Hermit
Pingback: What does Medical Hermit blog advice diligently about? - Medical Hermit
Pingback: Flexibility can give you pain; how can you find out excessive flexibility? - Medical Hermit
Pingback: How to manage Rheumatoid Arthritis? Rapid Jumpstart Advice - Medical Hermit
Pingback: What are harmful exposures for autoimmune arthritis? Quick guidance on 2 main ones. - Medical Hermit
Pingback: Acupuncture for pain relief in 3 main Rheumatological diseases. Quick guidance. - Medical Hermit
Pingback: When to immunosuppress Sjogren syndrome? Quick guidance on 5 points - Medical Hermit
Pingback: How to manage psoriatic arthritis and/or psoriasis? Quick effective guidance on 3 types of medications - Medical Hermit
Pingback: Ankylosing spondylitis diagnosis, HLA B27, and confirming it. Quick guidance - Medical Hermit