Introduction
I have to mention that I am not the expert that manages multiple sclerosis nor myasthenia gravis. However, due to getting large number of referrals for pain and whatever primary can not figure out, as a Rheumatologist, I started getting a sense when to consider them. I do not do the work up for them as they might entail nerve conduction studies, Magnetic resonance imaging, and spinal tap. All tests that can mainly be ordered by neurologist alone. I will discuss them at the end of the article briefly but let us have a talk about the history of the above three.
It is quite tricky to diagnose or suspect multiple sclerosis and myasthenia gravis. For one, they are rare. Second reason is that their tests are not readily available to primary providers. Let me start with simplified definition of each:
Fibromyalgia
Fibromyalgia: is a pain syndrome associated with other possibly other functional symptoms such as generalized weakness, headaches, mental fogginess, irritable bowel syndrome, and bladder spasms- to name a few. Look my article “Why is all my bones, muscles, and/or skin hurting?”. Disease main symptoms is diffuse pains. Typically, patients are in their 40’s or above. Typically, patients have history of a major social, psychological, physical, or medical stress.
Multiple sclerosis
Multiple sclerosis: is typically a disease were localized weakness, localized sensation loss, temporary vision loss, and instability on walking that comes and goes. Usually, these episodes could occur for few days once a month then disappear. Then symptoms return again. When I say localized, I mean one limb (arm or leg) or part of limb. This disease typically occur in young women.
Myasthenia gravis
Myasthenia gravis is a neurological disease that causes again weakness but seems predominantly in the head and neck area. These patients can get double vision (not blurry vision, double vision is seeing something twice), have difficulty swallowing food, or poor face muscle movements (look this website). This disease typically occur in young women or men older than 50.
In myasthenia gravis, patients would note that the more they move a muscle the more it becomes weaker. These muscle could be the jaw muscles when eating or the eyelid muscles. Or you can get progressive weakness of shoulders and hips, so wont be able to move arms above head or stand up from a chair, but keep in mind, this latter issue can be seen in other autoimmune muscle disease. These latter muscle disease are figured out also by measuring creatine kinase levels and you would see levels in 1000’s or more.
The confusing symptoms
The issue when you look online you will see MS, myasthenia gravis, and fibromyalgia has symptoms of headache, fatigue, and memory loss. These are horrible symptoms to base diagnosis off, as they are super vague and have a long list of reasons. The only one I, personally, would consider serious and pushing towards multiple sclerosis is forgetting pieces of information that you know that you know.
For example, if you are an engineer and you forget basic results of equations you use frequently, this is concerning. However, if you generally feel unable to focus and while thinking about something you lose track, I feel this goes towards fibromyalgia rather than MS or myasthenia gravis. Again, typically Multiple sclerosis and myasthenia gravis are acute to subacute meaning develop over months rather than years as fibromyalgia.
Neurologist evaluation
So what is the testing for MS and MG. First and foremost the main way is an evaluation by a neurologist and their physical exam. Then if the neurologist is suspicious enough, they will order nerve conduction study. This test uses needle to give and measure electricity of nerves and muscles. For MG, neurologist might do the test slightly differently to find the progressive weakness with recurrent stimulation. Magnetic resonance imaging of brain and spinal cord might be done to look for multiple sclerosis lesions.
Finally, for multiple sclerosis, the neurologist might recommend obtaining fluid from around your spinal cord called spinal fluids to see if there are white blood cells there or some form of antibodies in comparison to what you have in your blood stream. Classically myasthenia gravis patients have acetylcholine Receptor (AChR)-blocking Antibodies in their blood. As with other autoimmune disease, you can have the disease with negative testing. This last test in commercial lab companies is called “myasthenia gravis panel” but keep in mind that a professional neurologist is the gold standard not a blood test.
Summary
In summary, when looking at localized weakness and tingling, facial weakness, double vision, or temporary vision loss that develops over months, specially in the young, think of MS and MG. If symptoms are in years and not localized and more diffuse weakness and tingling, specially after age 40, think fibromyalgia. As I said above, diagnosis could be elusive.
Resources:
https://www.neurology.org/doi/10.1212/WNL.0000000000009238 (myasthenia gravis)
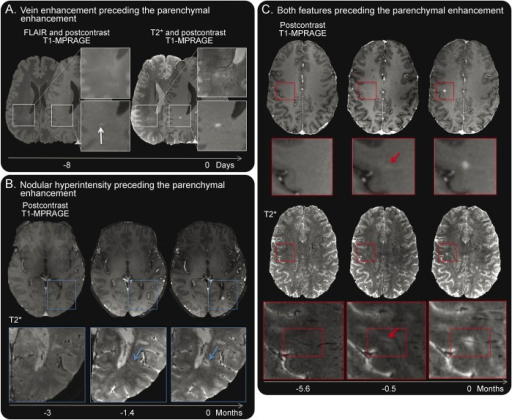
Absinta M, Nair G, Sati P, Cortese IC, Filippi M, Reich DS -Neurology® neuroimmunology & neuroinflammation(2015) https://creativecommons.org/licenses/by-nc-nd/4.0/



