List of joints to help you understand more
When I say joints, I mean any part of your body that bends. Before discussing type of arthritis let us talk joints. For me I list them as following: far finger knuckles (DIP), middle finger knuckles(PIP), knuckles where fingers attach to hand (MCP), base of thumb close to the wrist(first CMC), wrists, elbows, shoulders, neck (cervical spine), back of chest(thoracic spine), lower back (lumbar spine), back of hip or buttocks (sacroiliac joint), hip proper (feel it in the groin and called femoroacetabular joint), knees, ankles, knuckles where toes attach to foot (MTP), and middle knuckles of toes (PIP). There are many more joints than that and more technically in the spine. But for the sake of future discussion of diagnosis (figuring out what you have) and treatment I chose these joints.
Distribution of joint/tendon pain matters
Why did I list these joints? Because some joint diseases prefer different joints to attack or harm. Although this is not the main manner, I figure out what is hurting your joints, but it adds to the info. Prior to delving into the categories of joint pain causes, let me talk about tendons which are wires connecting muscles to bone to help move joints. These tendons can get hurt a lot when specific groups of muscle moving them get weak. The weaker the muscle, the more load is on the tendon and joint. Also let us mention the word bursa which I will describe as a ball that the tendon lubricates on. BUT if there is too much load on the tendon these balls(bursa) get irritated too. The common tendon bursa combination I deal with in my clinic are the internal shoulder muscles (rotator cuff muscle and subacromial bursa) and the hips side pain (trochanteric bursitis). The first one is due to the weakness of rotator cuff that stabilizes the shoulder joint. The second is due to weakness of a muscle called gluteus Medius which gets weaker as we tend to ignore it when we exercise. I will dedicate some brief explanation of exercises to reduce the chances of tendon and joint damage.
Main differentiating question for type of arthritis
So how do I diagnose typically the reason of your joint/tendon pains. For a Rheumatologist we have two main categories for specific joint pains. The one that is way more common, I will call it mechanical. I mean by that from overuse or misuse of your joints and tendons, they wear out. When joints wear out, we call them OSTEOARTHRITIS. At this point in time, there is no pill that reduces the progression (getting worse) of the damage. BUT exercise, weight loss, physical therapy, and dealing with metabolic disease (such as diabetes) can slow down the process. If all humanity lived to 120, we probably all would get OSTEOARTHRITIS. If tendons wear out, we call it tendinopathy. Typically, pain gets progressively through the day and when a person is ready to get to bed. Then when you wake up you are somewhat better. You might not be able to move the joint for some time up to 1 hour, especially if you have osteoarthritis for a while, which I typically see at ages 50 and above.
When is it autoimmune/inflammatory arthritis?
The other category of joint issue is inflammatory. Ok the word inflammation is quite confusing. At times, I feel that even seasoned professors confuse it. The word inflammation is commonly mistaken and confused for pain attack, swelling, tingling feeling, or just any plain uncomfortable sensation. If you want to confuse your primary health care provider and increase chances of getting a wrong diagnoses and more unnecessary testing then tell them “I am inflamed and stiff” without any further discussion. You will end up on a loop of doctor-to-doctor referral and could delay your diagnosis up to years. “doc, what do you mean inflammatory arthritis/arthropathy?” in my mind they can have 2 flavors. The first flavor has 3 traits. Trait one is inability to move the joint for 2-3 hours when you wake up for your day. Trait two, you feel much better as you move your joint almost all the time. Third trait, pain is typically way worse in the beginning of your day, but better in the middle of your day. A fourth, non-official characteristic is that low dose of prednisone 5-10 mg completely eradicates your pain in 1-2 days. Be careful that I said low dose NOT Medrol dose pack and NOT 60 mg. As high dose prednisone can resolve a lot of issues and is not an accurate tool to figure out things at this high dose. Response should almost always be immediate. The other flavor is what typically I see in a disease called gout. These patients will have sudden extremely painful pain in a specific joint to the degree you cannot even touch the joint. Even throw a sheet of paper on the joint will put that joint in agonizing pains. I have seen war veterans cry for the first 2 days of gout attack.
What joints typically affected in osteoarthritis or wear/tear arthritis
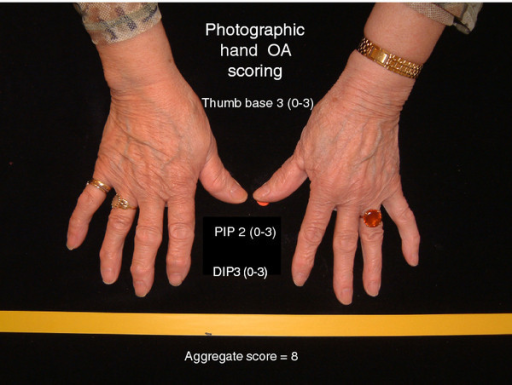
Now you might have a clue to what group of joint pain you have: mechanical vs inflammatory. “But doc, I kind of not sure even after reading what you said” At times you can have both kind of joint pain at the same time. TYPICALLY, THOUGH, inflammatory joint pains are more sudden in onset. Meaning they occur and develop in a short time such as 3 months while osteoarthritis you notice some pains then it gets bad in years after first time. Additionally, distribution of joints hurting can help. In general, although not always, Osteoarthritis causes damage to knees, hips, base of the thumb, far hand knuckles, middle finger knuckles, and spine. Inflammation joint pains involve knuckles of fingers where it attaches to hands, wrists, ankles, toes joints, and elbows. Ok there are exceptions of course. Let us say you are a dialyses nurse, you might get elbow pains and tendons around elbows pains due to carrying big jugs of electrolyte fluids. This is really a thing, and I am not faking a story. Ok another exception, I think is important to mention: If you are less than 40 and have lower back pain and you cannot explain it, then you might have inflammation of the spine and the buttocks joint which your primary can figure out with a magnetic resonance imaging (which is an expensive machine that you lay in and takes picture of you by measuring your magnetic activity).
Summary
In summary, most people belong to the osteoarthritis category that is better managed by dieting, exercise, physical therapy, and possibly over the counter medications. However, the Rheumatologist can help by giving injections to painful joints or tendons. The other group that is related to inflammation and these probably should see a Rheumatologist most times. For inflammatory/autoimmune joint disease, you would need some kind of medication to stop the disease and control your pain better. Further information on management of osteoarthritis and Rheumatoid arthritis, they will be discussed in future articles.

https://creativecommons.org/licenses/by-nc-nd/3.0
https://openi.nlm.nih.gov/faq#copyright
Zaniewicz-Kaniewska K, Sudoł-Szopińska I -Journal of ultrasonography(2013)
https://creativecommons.org/licenses/by/2.0
Jonsson H, Helgadottir GP, Aspelund T, Sverrisdottir JE, Eiriksdottir G, Sigurdsson S, Eliasson GJ, Jonsson A, Ingvarsson T, Harris TB, Launer L, Gudnason V -BMC musculoskeletal disorders(2012)




Comments
Pingback: Rheumatology evils: Anxiety/depression, poor diet, sloth, alcohol, and smoking. - Medical Hermit
Pingback: How to manage psoriatic arthritis and/or psoriasis? Quick effective guidance on 3 types of medications - Medical Hermit