Severe vs non-severe for the decision sjogren syndrome immunosuppressing
Let me define common issue before I delve and start talking about when to immunosuppress Sjogren syndrome. Like any disease, Sjogren syndrome has symptoms that are common and other that are rare. For rare issue, these individuals do not typically present to primary care clinic but rather the go to emergency department and get admitted. This leads to investigations of the issue.
Afterwards as docs are looking for reasons they investigate an array of common reasons. If none could be found, then autoimmune diseases are considered. If Sjogren syndrome was discovered, then docs then and there would provide aggressive therapy such as Rituximab, IVIG, and more rarely cyclophosphamide. All these are lupus meds mention on “how to treat lupus”. From my article “do I have Sjogren” you will know few issue that your primary wants you to see a Rheumatologist for.
When to suppress immunosuppress sjogren syndrome that is not severe?
Typically, a big question for a Rheumatologist in Sjogren syndrome is to immunosuppress or not to immunosuppress. Keep in mind that generally in absence of other underlying autoimmune disease, Sjogren syndrome patients has normal life span. Also, Sjogren does not damage joints. Rarely, does Sjogren affect nerves in a sense of small fiber neuropathy discussed in this article. Clinically, beside the rare dangerous stuff, I mentioned above, I usually consider my medications to prevent further salivary gland damage and reduce joint pains. Disclaimer, generally speaking I do not immunosuppress for fatigue as most our drugs could cause fatigue themselves.
When to immunosuppress for Sjogren syndrome dryness?
For the salivary gland protection, I am typically willing to try medications if dryness is less than 5 years old and more likely if less than 1 year old. If you have your disease diagnosed 20 years ago, usually whatever damage happens happened and we focus on symptom control. Last usually means keeping follow up with ophthalmologist, ENT, and/or dentists. For joint pain, I usually treat when pains sound autoimmune. I have described in my prior article when do I think joint pains are autoimmune but long story short when you have limited joint movements for 2 or more hours in the morning and/or pains getting better as days progresses.
Sjogren syndrome research protocol and how it helps in the decision
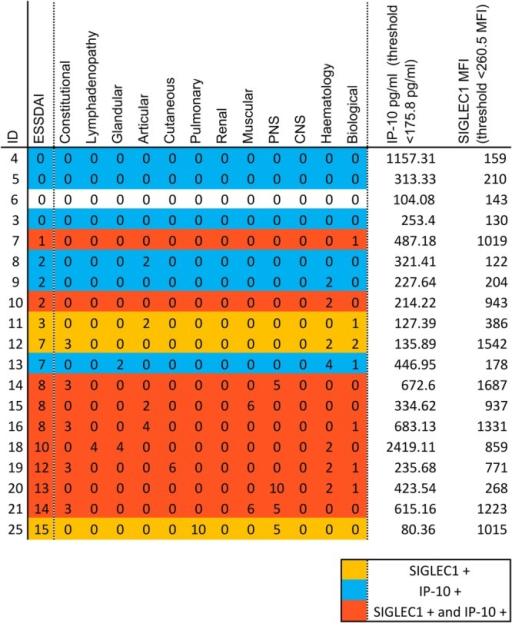
So going from when to treat, I like the way that Sjogren syndrome research people do it. To qualify for new Sjogren medication trials, usually symptoms should have started less than 5 years ago. Also, they use a score called ESSDAI score. I am not going to go through all of it as some parts of it is commoner than others. Keep in mind though, most these symptoms are issues that can be seen in other disease, therefore as your providers, we MUST make sure that you do not have other more common reasons for those issues.
The first is fever and weight loss with no explanation. When I hear fever, I think “make sure not infection” including long standing ones with fungi and parasites. When I hear weight loss, I think make sure not cancer or bowel issues preventing food absorption. Second, lymph nodes swelling, again with no other explanation. As discussed in “do I have Sjogren”, most times, we need lymph node biopsy to make sure there is no cancer. Third, swelling of salivary gland in the cheeks or under the jaw without other explanation. Again, as mentioned in “do I have Sjogren”, I usually need a biopsy.
What blood test could encourage me to immunosuppress sjogren syndrome?
OK what about blood testing. If you have low white cell count (cells that fight infections), low hemoglobin (substance in blood that carried oxygen), or low platelets (small floaty pieces of cells that helps with preventing bleeding) then I would consider treatment. I make sure there are no other reasons for that issue such as some viral infections (HIV) or vitamin/micronutrient deficiencies. Some kind of test called complements (C3 and C4) being low, although we keep in mind lupus more commonly when we see this.
Finally on a test SPEP/UPEP or measured specifically we could see high immunoglobulins indicating that B cells (kind of white cells) are overactive. Keep in mind all these tests are not diagnostic (meaning for sure is) but if a Rheumatologist is sure, you have Sjogren, then it kind of make sense to blame it as long as: you reasonably make sure no other issues going on.
Brief on medication used to immunosuppress sjogren syndrome
For the types of medications available you can look at how to treat lupus but in general medications are hydroxychloroquine, Azathioprine, and/or Methotrexate for simple cases. For more complex issues Rituximab, IVIG, or even cyclophosphamide is considered.
Resources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4613159
RMD Open https://creativecommons.org/licenses/by-nc/4.0/



